The retina and vitreous are subject to a wide range of degeneration’s and diseases, most of which can be successfully treated, especially with early diagnosis.
Retina
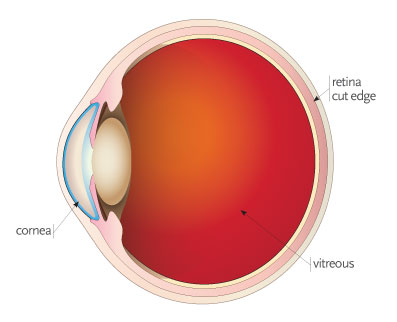
The retina is a thin, delicate tissue that lines the back wall of the eye. The retina is responsible for converting and decoding the light that is focused by the eye into tiny electrical impulses that can be transported to and interpreted by the brain. Without a functioning retina, vision is not possible.
-
What is Vitreous
The vitreous is a jellylike material that fills the central compartment of the eye. It plays an important role in helping maintain the optical clarity of the eye.
-
Diagnosing Retinal Diseases
The retina and vitreous are subject to a wide range of degenerations and diseases, most of which can be successfully treated, especially with early diagnosis. Retinal conditions can be diagnosed only by a thorough eye examination that includes the dilation of the pupil. Trained and skilled in the health of the eye, your surgeon can determine whether a retinal condition or other eye disorder may be affecting your vision. In an eye examination, the total health of your eyes, as well as the condition of your eyesight, is thoroughly examined. First and foremost, your visual acuity is checked to determine your current level of vision. Next, a slit lamp is used to look inside your eye. Following dilation of the pupil with eye drops, various instruments are used that allow the doctor to closely examine the structure of the retina. Other testing devices may be used to help determine the extent to which retinal disease may be present.
YOUR SURGEON STRIVES TO PRESERVE YOUR EYESIGHT AND SLOW THE PROGRESSION OF THE DISEASE.
What are some common conditions that affect the human retina?
-
Diabetic Retinopathy
Diabetes mellitus (DM) is a disease that affects blood vessels throughout the body, particularly vessels in the kidney and in the eye. When the blood vessels of the eye are affected, the condition is called diabetic retinopathy. Diabetes mellitus causes these blood vessels to leak fluid and blood into the retina, disturbing the normal architecture of the retina.
Diabetic retinopathy is the leading cause of new blindness among adults in the United States. If untreated there is a risk of becoming blind. The longer one has DM, the higher the incidence of developing diabetic retinopathy. Approximately 80% of people who have had DM for 15 years or longer have some damage to their retinal vessels. With adequate medical control and today’s treatment, only a small percentage have serious vision problems.
There are two stages of diabetic retinopathy. The first stage is background diabetic retinopathy and the second (later) stage is proliferative diabetic retinopathy. Background diabetic retinopathy is associated with leakage and bleeding within the retina. Diabetes causes retinal blood vessel walls to become incompetent, leading to fluid buildup within the retina. Vision may be unaffected or significantly reduced. If enough retinal blood vessels are destroyed by diabetes, the retina may respond by growing new blood vessels; this is called proliferative diabetic retinopathy. The vitreous can then fill with blood, leading to rapid vision loss. These new vessels can also promote scarring on the surface of the retina, leading to traction and retinal detachment. Both stages of diabetic retinopathy can lead to severe vision loss and need to be diagnosed right away. In many cases, treatment is needed to prevent or minimize vision loss. Persons with diabetes should have regular examinations with their primary eye doctor to diagnose these conditions before permanent vision loss sets in.
-
Macular Degeneration
Macular degeneration is the disease that affects the center of the retina, called the macula. The macula, which is about the size of the capital letter “O” in this sentence, is the part of the retina that is capable of our most detailed vision. We use the macula for reading, driving, recognizing faces, watching television, and performing fine work. Macular degeneration is the leading cause of legal blindness in people older than 55 (legal blindness means that a person has ≤20/200 visual acuity with eyeglasses). Even with a loss of central vision, color vision and peripheral vision may remain clear in persons with macular degeneration. There are two basic forms of the disease: wet and dry. The wet form affects one eye at a time and can result in sudden vision loss. The dry form affects both eyes, gradually disrupting central vision.
Some common symptoms of macular degeneration are distorted vision, gradual loss of color vision, the ability to see objects clearly, and the appearance of a dark or empty area in the center of vision. Central vision that is lost to macular degeneration can rarely be restored.
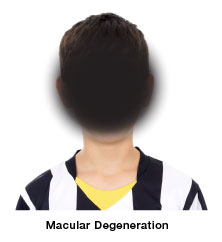
AGE-RELATED MACULAR DEGENERATION SYMPTOMS INCLUDE LOSS OF CENTRAL VISION, BLIND SPOTS OR STRAIGHT LINES AND FACES APPEARING WAVY.
Recent studies indicate that certain vitamins and minerals may help prevent or slow the progression of macular degeneration. Currently, scientists are undertaking the research necessary to determine the causes of macular degeneration. Finding the cause is the first important step toward prevention and cure. After age 50, an annual comprehensive eye examination is important to maintain eye health.
New advances have made treatment of macular degeneration possible. Laser treatment, photodynamic therapy, and novel medications contribute to successful treatment. In addition to medical and laser treatment, low-vision devices such as telescopic and microscopic lenses can be prescribed to maximize a person’s remaining vision.
FLASHES AND FLOATERS CAN BE AN INDICATION OF A POTENTIALLY SERIOUS PROBLEM WITH THE RETINA. ONLY A DILATED RETINAL EVALUATION CAN RULE OUT A SIGNIFICANT PROBLEM.
-
Flashers and Floaters
Flashes appear as flashing lights or as “lightning strikes” in the field of vision, although no light is actually flashing. Flashes are similar to the sensation of “seeing stars” when one is hit on the head. Flashes are most often noticed at night or in a dark room.
A floater is a small clump of gel that forms in the vitreous, which is the clear jellylike fluid that fills the cavity inside the eye. Floaters may be seen as dots, lines, cobwebs, or spiders and are most often noticed when reading, looking at a blank wall, or gazing at a clear sky. Although floaters seem to be in front of the eye, they are actually floating in the fluid inside the eye. Sometimes floaters do not interfere with vision at all. However, when a floater enters the line of vision, light is blocked and a shadow is cast on the retina.
A new onset of flashes or floaters is cause for concern. The vitreous tends to become more liquefied as a person ages. This can lead to mild floaters in one or both eyes, called benign floaters. However, a sudden burst of flashes or floaters in one eye suggests that the vitreous is undergoing an acute change. If the vitreous liquefies sufficiently, the back portion of the vitreous can peel off the surface of the retina. This process (called vitreous detachment) may take up to a couple of weeks. During this time, if the vitreous has tight adhesion’s to the retina, the retina can tear while the vitreous is detaching. It is critical to see your surgeon to check for retinal tears because most develop during this 2-week period. Although flashes and floaters may not fully diminish after these 2 weeks, the risk of developing a tear is greatly reduced if these 2 weeks pass with the retina still intact. If a torn retina is diagnosed, immediate treatment is necessary. Whether the retina tears or not, most people find that their flashes and floaters gradually diminish over the course of weeks or months. In rare cases floaters can persist for longer periods.
-
Retinal Detachment
Retinal detachment occurs when the retina becomes separated from the back wall of the eye. When the retina becomes detached, the blood supply is reduced and its ability to process light rays is impaired. If total detachment occurs and is not repaired, the retina becomes useless (as it can no longer transmit information to the brain) and the eye becomes blind.
As part of the normal aging process, the clear fluid that fills the inner cavity of the eye (the vitreous) begins to shrink and pull away from the retina. Most of this shrinking causes no damage to the eye. However, if the vitreous remains attached to the retina, the shrinking of the vitreous will cause the retina to tear. These tears usually occur in the peripheral retina, where there is little effect on visual acuity. If left untreated, retinal tears can lead to retinal detachment. Once a retinal tear is present, fluid from the vitreous may seep through the tear into the space between the retina and the wall of the eye. The fluid causes the retina to separate from the back of the eye or detach. The part of the retina that becomes detached will not function properly, resulting in vision loss.
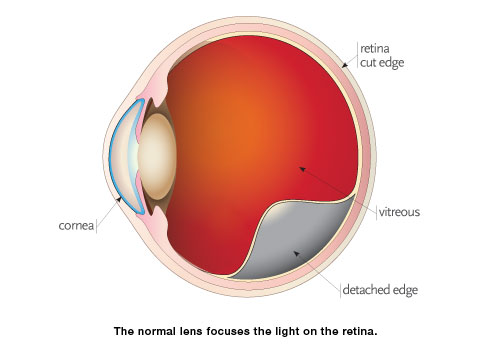
Retinal tears and retinal detachment are serious problems that require immediate treatment. Persons who are severely nearsighted or who have had a family history of retinal detachment should have regular eye examinations to detect any changes in the vitreous or in the retina. Persons who have experienced a serious eye injury should be examined for retinal damage. Persons with a sudden onset of flashes or floaters should be promptly examined. With early diagnosis retinal tears can be treated before retinal detachment and loss of vision occur. Retinal tears require immediate treatment to prevent retinal detachment and vision loss. Treatment of retinal tears is designed to create a scar that welds the retina to the back of the eye to prevent further tearing. The scar seals the tear and blocks fluid from passing under the retina. Retinal tears can be sealed using laser light or a freezing probe (cryopexy). During laser treatments, heat from the laser is used to place small scars around the edge of the tear to seal the break. With cryopexy, extreme cold is applied to the surface of the eye at the point of the tear to form a scar. Laser treatment and cryopexy are performed in the office.
Retinal detachments must be repaired surgically. In general, treatments should be prompt. Your surgeon will discuss the best treatment based on the location and extent of the retinal detachment. Most retinal detachments can be repaired with one procedure, while other retinal detachments require multiple surgical procedures. The total recovery time after retinal reattachment surgery can be weeks or months.


